Mucus Dysregulation in COPD and Asthma Causes Mucus Plug Formation and Airway Obstruction
The airways of the lungs are protected from environmental injury by a mucus gel comprised of mucin glycoproteins (“mucins”).1-7 In healthy airways mucus gel has low viscosity and elasticity and is easily transported by ciliary action. In muco-obstructive lung diseases, like COPD, oxidative stress can cause mucus gels to become pathologic via increased disulfide cross-linking. Increased viscosity and elasticity inhibit mucus gel transport, resulting in the formation of mucus plugs that obstruct airways.5,8
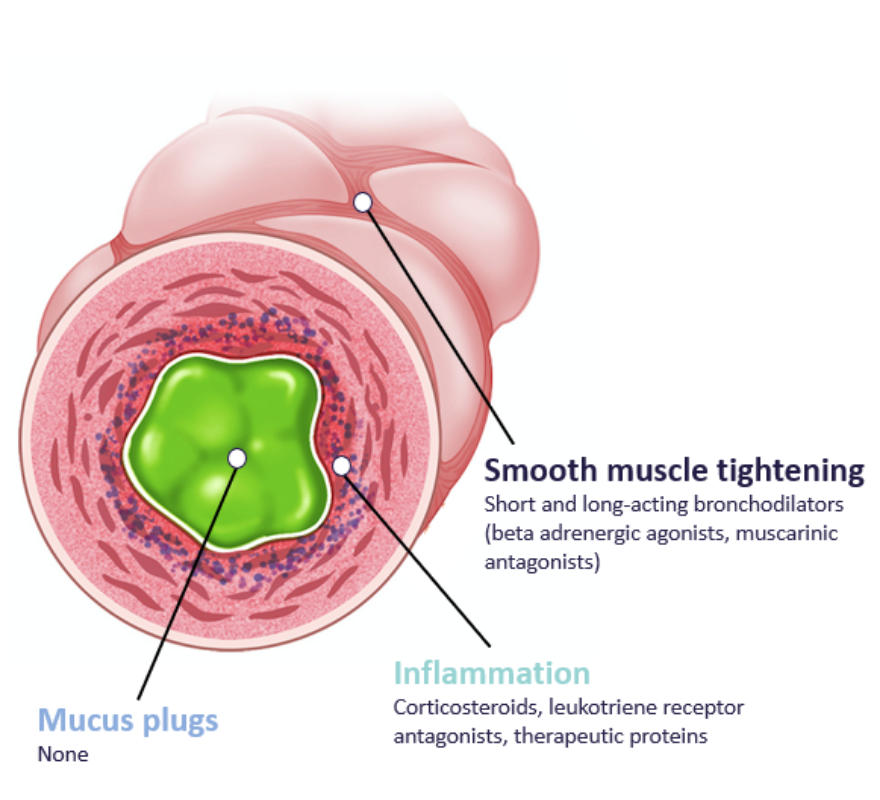
Current treatments for COPD and asthma have minimal effects on mucus, especially mucus plugs. The discovery that excessive disulfide bonds are a key mechanism of formation of pathologic mucus gels has led to the development of the thiol saccharide compound AER-01 as a novel mucolytic drug.
AER-01 Cleaves Disulfide Bonds in Mucus Plugs to Reduce Airway Obstruction
AER-01 is a thiol-modified carbohydrate (“thiol saccharide”) that works by cleaving disulfide bridges to liquefy (lyse) mucus plugs. It is highly soluble and well suited for delivery by nebulizer or dry powder inhaler.
Removing mucus plugs from the lungs will improve lung health. The specific clinical benefits include better lung function and lessening of symptoms of cough, shortness of breath, and chest congestion.

Targeted Development of AER‑01
Analysis of computed tomography (CT) lung scans from patients with COPD reveals a high prevalence of mucus plugs, especially in patients with more severe airflow obstruction. Specifically, a bronchopulmonary segment-based mucus plug score shows that 30-50% of COPD patients in GOLD stages III and IV (severe and very severe COPD) have high mucus plug scores.10 The mucus plug scoring system also reveals that mucus plugs in COPD patients are associated with increased frequency of exacerbations, high all-cause mortality, and accelerated decline in FEV1.10,11
The mucus plug score generated from analysis of CT lung scans will be leveraged in the clinical development of AER-01 as a predictive and monitoring biomarker of mucus plug burden in the lungs.
The mucus plug score generated from analysis of CT lung scans will be leveraged in the clinical development of AER-01 as a predictive and monitoring biomarker of mucus plug burden in the lungs.
References:
1. Thornton DJ, Sheehan JK. From mucins to mucus: toward a more coherent understanding of this essential barrier. Proc Am Thorac Soc 2004;1:54-61.
2. Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest 2002;109:571-7.
3. Thornton DJ, Rousseau K, McGuckin MA. Structure and function of the polymeric mucins in airways mucus. Annu Rev Physiol 2008;70:459-86.
4. Rose MC, Voynow JA. Respiratory tract mucin genes and mucin glycoproteins in health and disease. Physiol Rev 2006;86: 245-78.
5. Cone RA. Barrier properties of mucus. Adv Drug Deliv Rev 2009;61:75-85. 6. Hattrup CL, Gendler SJ. Structure and function of the cell surface (tethered) mucins. Annu Rev Physiol 2008;70:431-57.
7. Linden SK, Sutton P, Karlsson NG, Korolik V, McGuckin MA. Mucins in the mucosal barrier to infection. Mucosal Immunol 2008;1:183-97.
8. Innes AL, Woodruff PG, Ferrando RE, et al. Epithelial mucin stores are increased in the large airways of smokers with airflow obstruction. Chest 2006;130:1102-8.
9. Yuan et al. Science Translational Medicine 2016.
10. Dunican, EM et al. Mucus plugs and emphysema in the pathophysiology of airflow obstruction and hypoxemia in smokers. Am J Respir Crit Care Med Vol 203, Iss 8, pp 957–968, Apr 15, 2021.
11. Diaz A. Mucus plugs occluding COPD airways: A review of their clinical impact. The 2023 International Workshop on Pulmonary Imaging.
